The evidence behind why we need a more modern, high-quality and responsive long-term care system.
The evidence behind why we need a more modern, high-quality and responsive long-term care system.
One in 5 seniors over the age of 80+ have complex care needs that require long-term care, but our system was not built for current or future care needs.
Today, nearly 48,000 people are waiting for long-term care. This waitlist has doubled over the past 10 years and it is expected to grow, likely surpassing 50,000 people in 2025.
Plus, long-term homes do not have enough staff because of the health human resources crisis happening across the broader health system and around the world.
We need to revitalize long-term care to meet the complex care needs of our growing seniors’ population. Below is the data proving why.
1 in 13 Ontarians will be over the age of 80 by 2040.1
Ontario’s 80+ population is projected to more than double by 2040.1
Nearly 2 in 5 unpaid caregivers are distressed.3
In 2023-24, 43.7% of caregivers in Ontario reported having distress.3
Distressed caregivers report 40 hours per week on care, more than double those who are not distressed.3
Yet 1 in 5 seniors over the age of 80 has complex care needs that can only be safely met in long-term care.3
To address growing need, we must build more long-term care capacity, introduce specialized models of care, and increase the number of long-term care staff while continuing to expand across the broader seniors’ care continuum.
Nearly 50% more residents entering long-term care require higher levels of support than in 2011.4
This is the lowest in Canada and well below the national average of nearly 10%.
These residents often are in rural communities without access to extensive home care or live alone without informal caregiver support.3
Of those moving into long-term care homes:
Complex medical needs
3 out of every 4 people entering long-term care have 3 or more different medical conditions.5
Daily living support
89% of people entering long-term care need support with activities of daily living.4
Medications
Nearly 75% of people entering long-term care require eight different medications, with 30% requiring 13 or more.5
Cognitive impairment
72% of long-term care residents have moderate to severe cognitive impairment.4
Patients often have multiple conditions.
Innovative models of care are needed to meet the higher mix of acuity care needs of residents.
Nearly 48,000 people are currently waiting for long-term care. That’s more than the population of a mid-sized town in Ontario such as Bradford, Orillia, Stratford, Orangeville, or Leamington.6
More than half of seniors wait 126 days or more to access long-term care, with some waiting up to 2.5 years.7
Licensed long-term care homes
There are 615 licensed homes operating across Ontario providing care to residents.8
Spaces for residents
There are just over 76,000 available long-term care spaces for residents. These spaces are at full capacity.8
Ontario needs over 30,000 new long-term care spaces to serve the number of people currently on the long-term care wait list. We also need an additional 48,000 spaces by 2029 to meet the growing demand.9
Across Canada, job vacancy rates have increased by nearly 60% in the health care and social assistance sector in five years, from 3.2% in July 2019 to 5.1% in July 2024. Job vacancies have seen an 87% increase within the same time period.10
Over 100,000 people work in long-term care in Ontario.11 They include registered nurses; registered practical nurses; personal support workers; social workers; social activity staff; nutritional managers; chefs and food services workers; housekeeping, laundry and maintenance staff; and administrators.10
By 2029, Ontario long-term care homes will require at least 58,600 more nurses and personal support workers alone to meet increased hours of care and support residents in new long-term care spaces. 12
That is more than double the current nursing and personal support worker workforce.
The health human resources crisis is happening in Ontario, across Canada and around the world and affects all health sectors, including long-term care.
In 2024, 80% of long-term care homes report having difficulty filling shifts for registered practical nurses and 53% for registered nurses.
And, more than 40% report having difficulty filling shifts for personal support workers and their dietary teams.12
Ontario homes reported a significant turnover in leadership in 2024.
45% of homes saw a change in their Director of Care, Assistant Director of Care, or Administrator.12
Bold action is needed to address the health human resources crisis across the health system. It will take all health sectors working together, with government, to ensure our aging population receives safe, quality care.
They provide affordable housing, specialized care and living to more than 76,000 residents in 615 licensed long-term care homes.8
With an Ontario long-term care wait list of nearly 48,000 people6, the Ontario government is committed to serving even more seniors by modernizing 28,000 older long-term care spaces and constructing 30,000 new ones.13
In addition to the invaluable care and services long-term care homes offer to their residents, they also generate significant social and economic benefits to families and other caregivers, their communities and the broader health and social services system.
If long-term care homes are enabled to deliver the 58,000 new and redeveloped long-term care spaces promised by the government, they could:

Reduce caregiver burden and distress by more than 820,000 hours per week across the province.14

Additionally, if these caregivers can then return to the job market or increase their hours of work, this could create almost $24 million in income potential per week across the province.14
As a major employer and user of local businesses and services, long-term care homes support local economies:
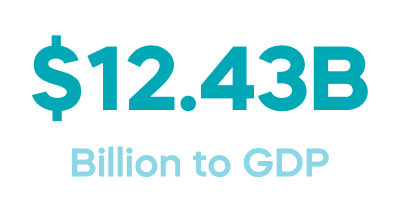
In 2024, long-term care homes contributed and/or supported $12.43 billion to GDP and $8.86 billion in labour income.14

In 2024, long-term care homes contributed 173,751 direct, indirect and induced jobs to Ontario.14
With nearly 48,000 seniors waiting for long-term care in Ontario6, we are seeing increased pressures in the community on supportive housing and assisted living, home care and community support services but complex health needs are going unmet.14
Meanwhile, long-term care homes create up to $100,000 in savings in the health system per day for every 100 alternative level of care patients who leave hospital and come to live in long-term care.14
Plus, the quality of life for those who move from hospital to a long-term care home improves significantly.14
*An ALC patient is someone who occupies a hospital bed because they need supports beyond what is available in their community or home but does not require the intensity of services provided in a hospital setting.
When we invest in long-term care, we invest in families, workers, seniors and the future of our province.
In the next 10 years, based on seniors’ population growth, the demand for long-term care is projected to increase by an average of 38%.9
By 2029, Ontario would require over 30,000 new long-term care spaces in order to serve our growing aging population.9
To learn about the challenges to redevelop and build new spaces in long-term care, visit our section on building and redevelopment.
The demand for long-term care will vary by region in Ontario.
Some regions in Ontario will have a higher demand for long-term care spaces in 10 years.9
Nearly half of Ontario’s long-term care homes need to be redeveloped to meet current demand.
To redevelop, long-term care homes need faster provincial and municipal approvals and stabilized operating funding so they can secure the confidence of their capital lenders. Plus, small, rural homes need capital programs tailored to their very unique needs.
Until recently, one of the missing pieces of information in our conversations about future seniors’ care planning was how well the Baby Boom generation is preparing for potential challenges as they age. As the oldest of the Boomers approaches 80, we wanted to know how they are preparing for the next stage of their life; what they think about their future care needs; and what plans they are putting in place.
In May of 2023, the Ontario Long Term Care Association commissioned Abacus Data to survey 1,000 Ontario residents aged 68 to 76 to help with our planning for the future.15
1 Ontario Data Catalogue, Population projections, accessed December 2024.
2 Ontario Caregiver Organization, Spotlight Report, December 2024.
3 Canadian Institute for Health Information (CIHI), Your Health System, accessed December 2024.
4 Canadian Institute for Health Information. Quick Stats, accessed December 2024.
5 Intellihealth, CCRS main and assessment package 2022/23 data, data retrieved December 2023.
6 Ontario Ministry of Long-Term Care Client Profile Database (CPRO), September 2024.
7 Ontario Health, Wait Times for Long-Term Care, accessed March 2024.
8 Ontario Ministry of Long-Term Care Inspector’s Quality Solution (IQS) Database, October 2024.
9 Preyra Solutions Group (PSG).
10 Statistics Canada, Job vacancies, payroll employees, and job vacancy rate by industry sector, monthly, adjusted for seasonality, Table 14-10-0406-01, data released January 25, 2024.
11 Ontario Long-Term Care Staffing Study, July 30, 2020.
12 Ontario Long Term Care Association (OLTCA), internal analysis, Fall 2024.
13 Ontario Ministry of Long-Term Care, News Release, Ontario on Track to Build 30,000 New Long-Term Care Beds, April 21, 2022.
14 Ontario Long Term Care Association (OLTCA), Provincial Snapshot: Socioeconomic benefits of long-term care, August 2024.
15 Abacus Data survey of 1,000 Ontarians aged 68-76, May 2023.